📅 Published on: July 15, 2024 | 🔄 Updated on: December 22, 2025 | By: Stem Cell Care India
Key Takeaways
- Reduces Gut Inflammation Stem cell therapy helps reduce strong inflammation in the colon. It calms irritated gut tissues quickly and naturally. The cells move to damaged areas and release healing signals. This helps reduce swelling and discomfort. As inflammation goes down, symptoms become easier to handle. The gut feels more stable and less reactive. With time, digestion improves, and sudden symptom rise become less frequent.
- Repairs Damaged Colon Tissue Stem cell therapy supports natural repair of the colon lining. Stem cells replace weak or damaged cells with healthy ones. It helps strengthen the colon walls. Better tissue repair reduces pain and bleeding. It also improves nutrient absorption. Over time, the colon becomes healthier and stronger. Slow healing brings long-term support for gut function.
- Supports Immune System Balance Stem cells help control an overactive immune system. They calm harmful immune attacks on the gut lining. This brings better immune balance in the body. With a balanced immune system, flare-ups reduce. Symptoms become milder and easier to manage. The therapy supports lasting immune stability. This helps patients feel steadier and more confident.
- Improves Quality of Life Stem cell therapy improves daily comfort. It helps reduce frequent bathroom visits. Patients feel less pain, less urgency, and better digestion. Energy levels rise as symptoms settle. Emotional stress also decreases with better control. Daily tasks become easier and more predictable. Overall quality of life improves as the gut becomes healthier.
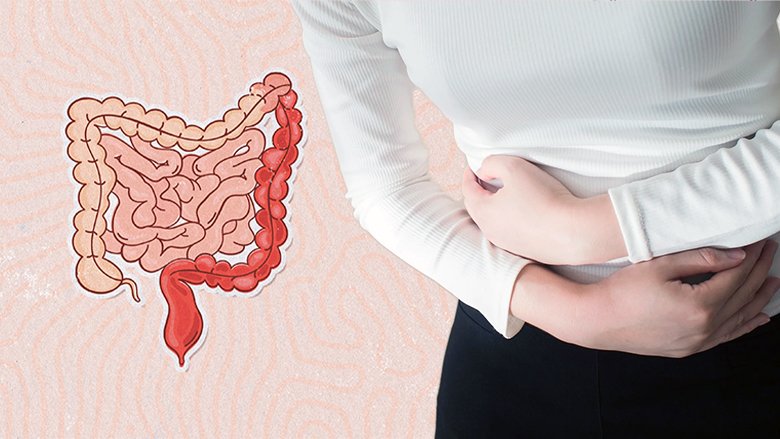
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that affects the large intestine (colon) and rectum, causing symptoms like abdominal pain, diarrhea, and rectal bleeding. Current treatments primarily aim to reduce inflammation and manage symptoms through medications like corticosteroids, immunomodulators, and biologics. However, for some patients who do not respond well to conventional therapies or suffer from severe disease, stem cell therapy has emerged as a potential alternative.
Stem cell therapy involves using stem cells to repair damaged tissues and modulate the immune response. Mesenchymal stem cells (MSCs) are particularly promising for UC treatment due to their ability to reduce inflammation and promote tissue repair. MSCs can be derived from various sources such as bone marrow, adipose tissue, or umbilical cord tissue. In UC, MSCs are believed to exert their therapeutic effects by suppressing aberrant immune responses and promoting mucosal healing in the colon.
Clinical studies exploring the use of MSCs in UC have shown encouraging results, although research is still in its early stages. These studies typically involve injecting MSCs directly into the affected areas of the colon or administering them intravenously. The goal is to achieve long-term remission by modulating the immune system and repairing damaged intestinal mucosa. While initial findings are promising, more extensive randomized controlled trials are needed to establish the safety, efficacy, and long-term outcomes of stem cell therapy for UC.
Stem cell therapy represents a potentially transformative approach in the treatment landscape of ulcerative colitis, especially for patient’s refractory to conventional therapies. By harnessing the regenerative and immunomodulatory properties of stem cells, researchers aim to not only alleviate symptoms but also induce long-term remission and improve quality of life. As ongoing research continues to refine techniques and validate outcomes, stem cell therapy holds promise as a future therapeutic option for managing this challenging inflammatory bowel disease.
Symptoms of ulcerative colitis (UC) can vary in severity and may fluctuate over time. Here are the key symptoms typically associated with UC: Given below are some of the common symptoms of ulcerative colitis:
- Diarrhea: Persistent diarrhea is a hallmark symptom of UC, often accompanied by urgency and the inability to control bowel movements.
- Abdominal Pain: Cramping and discomfort in the abdomen, especially in the lower left side, are common. Pain severity can vary from mild to severe.
- Rectal Bleeding: Blood in the stool is a frequent symptom, ranging from mild traces to significant bleeding. It may present as bright red blood or as darker, tarry stools.
- Urgency: The sudden and intense need to have a bowel movement, which can be difficult to control, is a characteristic symptom.
- Fatigue: Chronic inflammation and frequent bowel movements can lead to fatigue and a general feeling of tiredness.
- Weight Loss: Loss of appetite, coupled with nutrient malabsorption due to inflammation, can result in unintended weight loss.
- Fever: Some individuals may experience low-grade fevers during flare-ups, which indicate increased inflammation.
- Joint Pain: Inflammation associated with UC can also affect joints, causing pain and swelling, especially in large joints like the knees.
- Skin Problems: Certain skin conditions such as erythema nodosum (painful red nodules on the skin) or pyoderma gangrenosum (painful ulcers) may occur in conjunction with UC.
- Eye Inflammation: Inflammation of the eyes (uveitis) can cause redness, pain, and blurred vision in some UC patients.
- Reduced Quality of Life: The chronic nature of UC and its symptoms can significantly impact daily activities, work, social interactions, and emotional well-being.
It’s important to note that symptoms can vary widely among individuals with UC. Some may experience mild symptoms that only flare up occasionally, while others may have more severe symptoms that require intensive medical management. Regular monitoring and communication with healthcare providers are crucial to managing UC effectively and improving the quality of life for patients.
Finding out the symptoms early can ease the diagnosis. It will also help doctors to provide the best treatment that suits your problems. If you are facing any of the above symptoms, then you should take a consultant from Stem Cell Care India.
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) characterized by chronic inflammation and ulceration in the inner lining of the colon and rectum. There are several types of UC based on the extent and location of inflammation within the colon. Given below are some of the common types of ulcerative colitis:
- Proctitis: This is the mildest form of UC and involves inflammation limited to the rectum (the lower part of the large intestine). Symptoms may include rectal bleeding, urgency, and tenesmus (the sensation of needing to pass stools even when the bowel is empty). People with proctitis may not experience diarrhea or abdominal pain as severely as those with more extensive forms of UC.
- Proctosigmoiditis: In this type, inflammation extends beyond the rectum into the sigmoid colon, which is the part of the colon just above the rectum. Symptoms typically include bloody diarrhea, abdominal cramps, urgency, and tenesmus. Individuals may experience more frequent and urgent bowel movements compared to proctitis alone.
- Left-sided colitis: This type of UC affects the left side of the colon, extending from the rectum up through the sigmoid and descending colon. Symptoms include bloody diarrhea, abdominal cramping, urgency, tenesmus, and sometimes weight loss and fatigue. Left-sided colitis can cause significant discomfort and disruption in daily life.
- Pancolitis: Also known as extensive colitis or total colitis, pancolitis involves inflammation that affects the entire colon, from the rectum to the cecum (where the colon joins the small intestine). Symptoms are typically severe and may include frequent bloody diarrhea, abdominal pain and cramping, fatigue, weight loss, fever, and dehydration. Individuals with pancolitis may be at higher risk for complications such as toxic megacolon (severe dilation of the colon), which requires urgent medical intervention.
- Fulminant colitis: This is a severe form of pancolitis characterized by sudden and intense symptoms such as severe abdominal pain, profuse diarrhea with bleeding, dehydration, fever, and rapid weight loss. Fulminant colitis is considered a medical emergency and requires immediate hospitalization and intensive treatment, often including intravenous fluids, corticosteroids, and sometimes surgery.
It’s important to note that the severity and extent of UC can vary over time, with periods of remission (when symptoms improve or disappear) alternating with flare-ups (when symptoms worsen). Some individuals may progress from a milder form of UC to a more extensive type throughout their disease. The exact cause of UC is not fully understood, but it involves a complex interaction between genetic predisposition, environmental factors, and an abnormal immune response targeting the intestinal lining.
Treatment approaches for UC depend on the type and severity of the disease and may include medications to reduce inflammation (such as aminosalicylates, corticosteroids, immunomodulators, and biologics), dietary modifications, lifestyle changes, and in severe cases, surgery to remove the affected colon (colectomy).
Ulcerative colitis (UC) is a complex condition believed to result from a combination of genetic, environmental, immunological, and microbial factors. While the exact cause remains unclear, several factors are thought to contribute to the development of UC:
- Genetic Predisposition: Individuals with a family history of UC are at a higher risk of developing the disease. Multiple genes have been implicated in UC, affecting the immune system’s ability to regulate inflammation in the intestines. Genetic studies have identified various susceptibility loci, but no single gene is solely responsible for UC.
- Immune System Dysfunction: UC is classified as an autoimmune disease, where the immune system mistakenly attacks healthy tissues in the gastrointestinal tract. In UC, immune cells accumulate in the lining of the colon and rectum, leading to chronic inflammation and tissue damage. Abnormal immune responses to gut microbiota or environmental triggers may trigger and sustain this inflammatory process.
- Environmental Factors: Environmental factors likely play a role in triggering UC in genetically susceptible individuals. Factors such as diet, stress, smoking, medications (e.g., nonsteroidal anti-inflammatory drugs), and infections may influence the onset and progression of UC. Changes in lifestyle or exposure to certain environmental triggers may also exacerbate symptoms during flare-ups.
- Gut Microbiota Imbalance: The gut microbiota, consisting of trillions of bacteria and other microorganisms, plays a crucial role in maintaining intestinal health and regulating immune responses. In individuals with UC, there appears to be an imbalance (dysbiosis) in the composition and function of gut microbiota. This dysbiosis may contribute to chronic inflammation and disease progression.
- Epigenetic Factors: Epigenetic modifications, which alter gene expression without changing the underlying DNA sequence, have been implicated in UC. These modifications can influence how genes related to immune function and inflammation are activated or silenced, potentially affecting disease susceptibility and severity.
- Barrier Dysfunction: Dysfunction of the intestinal epithelial barrier, which normally protects against harmful substances and regulates immune responses, is observed in UC. Genetic and environmental factors can compromise barrier function, allowing bacteria and other antigens to penetrate the intestinal lining and trigger an inflammatory response.
While these factors are recognized as potential contributors to UC, the interplay between genetics, environment, immune response, and gut microbiota remains an active area of research. Understanding these underlying mechanisms is critical for developing more targeted therapies and interventions to manage and ultimately prevent UC.
Diagnosing ulcerative colitis (UC) involves a combination of clinical evaluation, imaging tests, endoscopic procedures, and laboratory tests to confirm the presence of the disease and determine its extent and severity. Here’s an overview of the diagnostic process for UC:
Clinical Evaluation:
- Medical History: A detailed history helps in understanding symptoms such as abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. It also includes questions about a family history of inflammatory bowel disease (IBD) and other relevant medical conditions.
- Physical Examination: A physical exam may reveal signs such as abdominal tenderness, palpable mass (in severe cases), and signs of dehydration or nutritional deficiencies.
Laboratory Tests:
- Blood Tests: Blood tests can indicate inflammation by measuring markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Blood tests also help assess nutritional deficiencies and screen for complications like anemia.
- Stool Tests: Stool samples may be analyzed for blood, infection, and inflammation markers (calprotectin) to differentiate UC from infections or other gastrointestinal conditions.
Imaging Studies:
- Endoscopy: Colonoscopy is the primary procedure for diagnosing UC. A flexible tube with a camera (colonoscope) is inserted into the rectum and advanced through the colon. This allows direct visualization of the colon’s inner lining to identify inflammation, ulcers, and the extent of involvement.
- Biopsy: During colonoscopy, small tissue samples (biopsies) are taken from the inflamed areas of the colon. Biopsies help confirm the diagnosis of UC and rule out other conditions such as Crohn’s disease or infectious colitis.
Imaging Tests:
- CT scan or MRI: These imaging tests may be used to assess the extent of inflammation, evaluate complications like abscesses or fistulas, and guide treatment decisions in severe cases.
Classification and Severity Assessment:
- Based on the findings from colonoscopy and biopsies, UC is classified into different types (e.g., proctitis, left-sided colitis, pancolitis). The severity of UC is often assessed using clinical criteria such as the Mayo score or endoscopic scoring systems.
Differential Diagnosis:
- It’s essential to distinguish UC from other conditions that cause similar symptoms, such as Crohn’s disease, infectious colitis, ischemic colitis, and colorectal cancer. This differentiation is crucial for appropriate treatment planning.
Monitoring and Follow-up:
After diagnosis, regular monitoring of symptoms, disease activity (through clinical assessment and laboratory tests), and surveillance colonoscopies are important to manage UC effectively and detect complications or disease progression early.
Treatment for ulcerative colitis (UC) aims to reduce inflammation, control symptoms, induce and maintain remission, and improve quality of life. The choice of treatment depends on the severity of symptoms, the extent of inflammation, and the individual’s response to previous therapies. Here are key approaches to managing UC:
First-line treatments often include medications such as aminosalicylates (e.g., mesalamine), which reduce inflammation in the colon and help control mild to moderate symptoms. Corticosteroids like prednisone may be prescribed for short-term use during flare-ups to quickly suppress inflammation, but they are not suitable for long-term maintenance due to side effects. Immunomodulators such as azathioprine, 6-mercaptopurine, or methotrexate may be used to suppress the immune system and maintain remission in moderate to severe cases or when aminosalicylates are ineffective. Biologic therapies, such as anti-TNF agents (e.g., infliximab, adalimumab), target specific proteins in the immune system to reduce inflammation and are often prescribed for patients who do not respond to other treatments. In severe cases or when complications arise, surgery to remove the affected portion of the colon (colectomy) may be necessary to alleviate symptoms and improve quality of life.
Stem cell therapy is still in its progressive state which means the outcomes will be different for each patient. Researchers are doing various clinical trials to make this treatment more effective. Initial findings indicate that it can help make things better for muscle weakness and thinking problems.
Stem Cell Care India offers a 3-day procedure to give you the best treatment for your condition. Given below are the procedures which include a number of tests, admission procedures, and many more:
Day 1-
- Pick up from the airport to the hospital.
- Interaction with doctor and patient, to clear all their doubts at that time.
- Admission procedure.
- Clinical examination & lab tests will be done as prescribed by the doctor
- Supportive therapy
Day 2-
- Stem cell procedure
- Supportive therapies
- Physiotherapy
Day 3-
- Supportive therapy
- Physiotherapy
- Discharging formalities
- Drop back to the airport
Note:
- For admission, carry the identity card (Passport/PAN card / Driving License)
- Carry the hard copy of patient reports
Implantation of stem cell treatment in ulcerative colitis (UC) refers to the process of administering stem cells into the body to treat the disease. Stem cell therapy for UC is an experimental approach aimed at harnessing the regenerative and immunomodulatory properties of stem cells to reduce inflammation and promote tissue healing in the colon.
- Types of Stem Cells: Mesenchymal stem cells (MSCs) are commonly used in stem cell therapy for UC. MSCs can be derived from various sources such as bone marrow, adipose tissue, or umbilical cord tissue. These cells can differentiate into different cell types and exert immunomodulatory effects, which are beneficial in dampening the abnormal immune response seen in UC.
- Administration: Stem cells can be administered through different routes depending on the specific protocol and study design:
- Local Administration: Stem cells may be directly injected into the affected areas of the colon during endoscopy or surgery. This approach allows for targeted delivery to areas of active inflammation.
- Systemic Administration: Stem cells can also be infused intravenously, where they circulate throughout the body and exert their effects on the immune system and inflammation systemically.
- Mechanism of Action: The exact mechanisms by which stem cells exert their therapeutic effects in UC are still being studied. However, potential mechanisms include:
- Immunomodulation: Stem cells can modulate the immune response, reducing inflammation and promoting tolerance to gut microbiota.
- Tissue Repair: Stem cells may promote tissue regeneration and repair of damaged intestinal mucosa, helping to restore normal barrier function in the colon.
- Anti-inflammatory Effects: MSCs can secrete anti-inflammatory factors and cytokines that counteract the inflammatory cascade seen in UC.
- Clinical Trials and Research: Clinical trials exploring the efficacy and safety of stem cell therapy for UC are ongoing. These studies aim to establish optimal protocols, determine long-term safety and efficacy, and identify patient populations most likely to benefit from this treatment approach.
- Challenges and Considerations: While promising, stem cell therapy for UC is still considered experimental and not yet widely available outside of clinical trials. Challenges include variability in patient responses, standardization of protocols, potential risks such as infection or immune reactions, and ethical considerations.
Implantation of stem cell treatment in ulcerative colitis represents an innovative approach with potential benefits in modulating the immune response and promoting tissue healing. Continued research and clinical trials are essential to fully understand its effectiveness, safety profile, and long-term outcomes for individuals with UC.
How does stem cell therapy work for ulcerative colitis?
Stem cell therapy, particularly using mesenchymal stem cells (MSCs), aims to modulate the immune system and promote tissue repair. MSCs can suppress inflammation, regulate immune responses, and stimulate healing of damaged intestinal mucosa. This process helps in reducing symptoms such as diarrhea, rectal bleeding, and abdominal pain, potentially inducing and maintaining remission in UC patients.
What are the sources of stem cells used in UC therapy?
Stem cell is used in ulcerative colitis treatment and can be sourced from a number of tissues, such as bone marrow, adipose tissue, and umbilical cord tissue. Each source has its own advantages and it may impact factors such as ease of harvesting, cell yield, and immunomodulatory properties. Researchers are exploring the optimal sources to maximize therapeutic benefits and minimize risks.
Is stem cell therapy safe for ulcerative colitis?
Current research suggests that stem cell therapy appears to be safe for ulcerative colitis when conducted under controlled conditions in clinical trials. However, like any medical intervention, there are potential risks such as infection, immune reactions, or long-term effects that require careful monitoring and evaluation. Clinical trials are essential to establish safety profiles and determine the best practices for using stem cell therapy in UC treatment.
What are the potential benefits of stem cell therapy over traditional treatments?
Stem cell therapy offers several potential benefits over traditional treatments for ulcerative colitis. These include its immunomodulatory effects, ability to promote tissue regeneration, potential for disease modification, and minimally invasive administration options. Unlike conventional therapies that primarily manage symptoms, stem cell therapy aims to address underlying disease mechanisms, potentially offering a more comprehensive treatment approach.
Is stem cell therapy currently available for ulcerative colitis outside of clinical trials?
As of now, stem cell therapy for ulcerative colitis is primarily investigational and not widely available outside of clinical trials or specialized treatment centers. Ongoing research is evaluating its efficacy, safety, optimal administration routes, and long-term outcomes. Patients interested in stem cell therapy should consult with healthcare providers and consider participating in clinical trials under the guidance of experienced medical professionals.
What symptoms can stem cell therapy help improve in UC?
Stem cell therapy may help reduce several UC symptoms. It can ease abdominal pain and calm gut inflammation. Many patients report fewer urgent bowel movements. It may also help lower bleeding and discomfort. Over time, the therapy supports better digestion. It focuses on healing the colon lining. This helps improve daily comfort and overall stability naturally.
How long does stem cell therapy take to show results?
Results can vary for each patient. Some may notice relief in weeks. Others may take months for visible improvements. Stem cells need time to repair tissues. They also work by calming immune reactions. Slow and steady healing supports long-term benefits. The timeline depends on symptom severity. Regular follow-ups help track progress better.
Can stem cell therapy reduce flare-ups in ulcerative colitis?
Yes, it may help reduce symptom-rise. Stem cells work by balancing the immune system. A calmer immune response means fewer sudden attacks. Reduced inflammation also lowers the risks. Over time, the colon becomes stronger. This helps create a more stable gut environment. Many patients experience longer periods of relief. Consistent care improves outcomes further.
Is stem cell therapy painful for ulcerative colitis patients?
The procedure is usually not painful. Most treatments use simple infusions. These are similar to regular IV drips. Patients often remain comfortable during the session. Minor discomfort may occur afterward. This is usually temporary and mild. There is no major downtime needed. Most people return to normal activity quickly.
How do stem cells support healing inside the colon?
Stem cells travel to damaged colon areas. They release natural healing signals. These signals calm inflammation gently. They help repair weak or irritated tissues. New healthy cells replace damaged ones. This improves the colon’s strength over time. Healing supports smoother digestion. It also helps reduce daily symptoms significantly.
Are lifestyle changes still needed after stem cell therapy?
Yes, lifestyle support remains important. A healthy diet helps manage symptoms. Stress control reduces gut irritation. Regular checkups keep progress on track. Stem cells improve healing, but habits matter too. Good sleep supports better immune balance. Gentle activity also helps overall health. Combined care brings stronger long-term results.
Who can be a suitable candidate for stem cell therapy?
Candidates include patients with moderate to severe UC. It helps those not responding well to medications. People seeking natural healing approaches may benefit. Doctors assess medical history and symptoms first. Suitability depends on overall health condition. Proper testing ensures safe treatment planning. A specialist decides the best approach for each patient.
After undergoing stem cell therapy for ulcerative colitis (UC), patients may experience several improvements in their condition, contributing to enhanced quality of life and overall well-being. Here are the key improvements commonly reported following treatment:
- Reduction in Symptoms: Many patients notice a significant reduction in UC symptoms such as diarrhea, rectal bleeding, abdominal pain, urgency, and tenesmus. These improvements are often indicative of decreased inflammation and improved mucosal healing in the colon.
- Remission Induction: Stem cell therapy has shown promise in inducing remission in UC patients who may not have responded adequately to conventional treatments. Remission means a decrease or absence of symptoms and can lead to prolonged periods of disease control.
- Decreased Dependency on Medications: Some patients may experience a reduced need for medications such as corticosteroids, immunosuppressants, or biologics after successful stem cell therapy. This reduction in medication dependency can mitigate associated side effects and improve long-term treatment adherence.
- Enhanced Quality of Life: Improvements in symptom control and disease management contribute to an enhanced overall quality of life for UC patients. They may experience less disruption to daily activities, improved sleep patterns, and better psychological well-being due to reduced disease burden.
- Long-term Disease Control: Stem cell therapy holds the potential for modifying the course of UC by addressing underlying disease mechanisms. This can lead to sustained disease control and fewer flare-ups over time, reducing hospitalizations and healthcare utilization.
- Tissue Healing and Restoration: Stem cells promote tissue repair and regeneration in the inflamed colon, helping to heal ulcerations and restore the integrity of the intestinal mucosa. This tissue healing process is critical for maintaining long-term remission and preventing disease progression.
It’s important to note that individual responses to stem cell therapy can vary, and not all patients may experience the same level of improvement. Ongoing research is essential to further elucidate the long-term efficacy, safety, and optimal use of stem cell therapy in the treatment of ulcerative colitis.
Stem cell therapy for ulcerative colitis (UC) involves complex mechanisms that contribute to its potential therapeutic effects. Here are the key mechanisms by which stem cells, particularly mesenchymal stem cells (MSCs), exert their actions in UC treatment:
- Immunomodulation: MSCs possess immunomodulatory properties that can regulate the immune response in UC. They interact with various immune cells such as T cells, B cells, and macrophages, suppressing pro-inflammatory responses and promoting anti-inflammatory pathways. This modulation helps to dampen excessive inflammation in the intestinal mucosa, which is a hallmark of UC.
- Anti-inflammatory Effects: MSCs secrete anti-inflammatory molecules such as cytokines (e.g., IL-10, TGF-beta) and growth factors that contribute to reducing inflammation. By altering the local immune environment in the colon, MSCs mitigate the immune-mediated damage to the intestinal epithelium seen in UC.
- Tissue Repair and Regeneration: MSCs have the capacity to differentiate into various cell types and promote tissue repair. In UC, chronic inflammation leads to ulceration and damage of the intestinal mucosa. MSCs contribute to tissue healing by stimulating epithelial cell proliferation, enhancing mucosal barrier function, and promoting angiogenesis (formation of new blood vessels).
- Induction of Regulatory T cells (Tregs): MSCs can induce the generation of regulatory T cells, which play a crucial role in immune tolerance and suppressing excessive immune responses. Tregs help maintain immune homeostasis in the gut and may contribute to long-term remission in UC patients treated with stem cell therapy.
- Antimicrobial Effects: MSCs have been shown to exhibit antimicrobial properties by enhancing the clearance of pathogens and promoting a balanced microbial environment (microbiota) in the gut. This antimicrobial effect is important in UC, where dysbiosis (imbalance in gut microbiota) is implicated in disease pathogenesis.
- Modulation of Fibrosis: In advanced stages of UC, fibrosis (excessive tissue scarring) can occur, leading to complications such as strictures. MSCs have been studied for their potential to modulate fibrotic processes and prevent or reduce the formation of fibrotic tissue in the colon.
Understanding these mechanisms is crucial for optimizing stem cell therapy approaches in UC, including determining the optimal cell source, dosage, timing of administration, and patient selection criteria.
Many people are suffering from ulcerative colitis and don’t get the right treatment for it. That’s why as the greatest healthcare consultant in India, we promise each and every patient to provide the best possible consultancy. So that they can get the best treatment according to their medical condition. Our commitment is to give each patient the best healthcare service by bringing them in place, providing them with stem cell treatment in recognized hospitals, and many more. Every individual trust us whether it is from India or over the sea. So, what are you waiting for? Take the best advice for your condition to get better treatment and live a happy and quality life.
The price of stem cell therapy in India is much less compared to other Western countries. Because we believe in providing the best treatment to each and every patient. Stem cell treatment is the hope of a number of patients and we don’t want our patients to not get it. However, the cost of stem cell treatment can’t get high but some factors influence it:
- First is the severity of the condition, if a patient’s condition is worse then it requires special treatment which can influence the cost.
- Past medical history can also raise the cost of the treatment because there could be a need for higher medication and measurement.
- Price can be determined if the patient’s BMI is not correct.
- There are also some other charges such as environmental factors, economic uncertainties, etc.
Stem cell therapy has a significant success rate because of its regenerative potential. Many people experience great improvement in their cognitive function. At the same time, some are getting their quality of life back. People are surprised how a treatment will be this good. And their answer is in their improvement. However, stem cell therapy is still in its experimental stage, so scientists are still researching it. A number of clinical trials and research are under process to make it more effective and beneficial for every patient. However, the success rate can depend on the patient’s age, the severity of the condition, and many more.
Stem cell therapy for ulcerative colitis (UC) offers several potential advantages, making it an attractive area of research and development in the treatment of this chronic inflammatory bowel disease:
- Immunomodulatory Effects: Mesenchymal stem cells (MSCs) possess unique immunomodulatory properties that can help regulate the abnormal immune response seen in UC. They can inhibit pro-inflammatory immune cells while promoting anti-inflammatory responses, thereby reducing inflammation in the colon. This modulation of the immune system may help induce and maintain remission in UC patients.
- Tissue Repair and Regeneration: MSCs have the ability to differentiate into various cell types and promote tissue repair. In UC, chronic inflammation leads to damage and ulceration of the intestinal mucosa. Stem cells can facilitate the regeneration of damaged tissues, promoting healing of ulcers and restoring the integrity of the intestinal barrier. This tissue repair process is crucial for reducing symptoms such as diarrhea, rectal bleeding, and abdominal pain.
- Minimal Invasiveness: Depending on the administration route, stem cell therapy can be minimally invasive. For instance, MSCs can be administered intravenously or directly into the affected areas of the colon during endoscopy. This approach avoids the need for extensive surgical procedures and may reduce recovery time and complications associated with more invasive treatments.
- Potential for Disease Modification: Unlike conventional therapies that primarily manage symptoms, stem cell therapy has the potential to modify the course of UC by addressing underlying mechanisms of disease pathology. By targeting inflammation and promoting tissue healing, stem cells may offer a more comprehensive treatment approach that goes beyond symptom control.
- Personalized Treatment Approach: Stem cell therapy holds promise as a personalized treatment option for UC. Research is ongoing to identify biomarkers and genetic factors that may predict patient response to stem cell therapy. This personalized approach could lead to tailored treatment plans that optimize therapeutic outcomes for individual patients.
- Combination Therapy Potential: Stem cell therapy can be used in combination with existing treatments for UC, such as immunosuppressants or biologics. This combination approach may enhance therapeutic efficacy and reduce the dosage requirements of conventional medications, potentially minimizing their associated side effects.
While these advantages are promising, it’s important to note that stem cell therapy for UC is still in the early stages of clinical research. Large-scale clinical trials are needed to establish safety, efficacy, optimal dosing regimens, and long-term outcomes.
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) affecting the colon, characterized by inflammation and ulceration of the inner lining. Effective quality control in managing UC revolves around several key principles.
Firstly, accurate diagnosis is crucial. This involves thorough clinical evaluation, including symptom assessment, imaging studies like colonoscopy, and histopathological confirmation via biopsy. Clear diagnostic criteria help ensure proper management from the outset.
Treatment planning in UC demands a multidisciplinary approach. Gastroenterologists, nutritionists, and sometimes surgeons collaborate to tailor therapies to the patient’s needs. Medications such as aminosalicylates, corticosteroids, immunomodulators, and biologics are used based on disease severity and response.
Monitoring disease activity and treatment response is integral. Regular assessments through clinical evaluations, laboratory tests (e.g., C-reactive protein), and imaging track progression and guide adjustments in therapy. This continuous evaluation minimizes disease flare-ups and optimizes patient outcomes.
Patient education is pivotal in UC management. Providing comprehensive information on the disease, treatment options, lifestyle modifications, and potential complications empowers patients to participate actively in their care. This enhances treatment adherence and promotes better health outcomes.
Adherence to evidence-based guidelines ensures consistency and standardization in care delivery. Guidelines from organizations like the American Gastroenterological Association (AGA) or European Crohn’s and Colitis Organization (ECCO) offer structured approaches to diagnosis, treatment, and monitoring, promoting best practices.
Lastly, ongoing research and professional development are vital. Keeping abreast of emerging therapies, diagnostic technologies, and management strategies through conferences, literature reviews, and clinical trials fosters continuous improvement in UC care.
Quality control in ulcerative colitis management hinges on precise diagnosis, multidisciplinary collaboration, vigilant monitoring, patient empowerment, adherence to guidelines, and ongoing education and research. These facets collectively ensure optimized outcomes and improved quality of life for individuals living with UC.
Patients are finding a number of improvements in their bodies after taking stem cell therapy for ulcerative colitis. As you know, stem cell therapy is one of the best treatment options and is good among patients. Stem cells are used in this therapy and can be differentiated into different types of specialized cells. Each specialized cell can help to repair the damaged cells and take its place. Which, patients can experience a number of benefits such as a reduction in inflammation, and many more. Stem cells are natural building blocks of your body that can treat several medical conditions without any side effects.
I suffered from ulcerative colitis, which was an extremely serious condition. I am not capable of doing things by myself. I went to all the doctors and they all told me the same thing: there is no cure. After I gave up, a friend advised me to contact Stem Cell Care India one of the best consultants in India, regarding your issue. I made an appointment by calling them. They help me in a variety of ways. They treated my condition, and for that, I was really grateful. —- Piyush Singh, India.
I had assumed that there was no cure for ulcerative colitis until I had a meeting with an excellent consultant at Stem Cell Care India. They are incredible and made treating my condition easier for me. They helped me a great deal by giving me advice and responding to my inquiries. I am living my life and am in perfect shape now. —- Nish John, South America.
I am so glad I found Stem Cell Care India. They offer me the best medical advice regarding my ulcerative colitis. I did not receive the proper treatment for this condition, which I had been experiencing for the past few months. It was a fantastic medical strategy that their team of doctors recommended that I take stem cell therapy. My body improved in a number of ways, and my inflammation decreased. — Ferb Joseph, South Africa.
I visit Stem Cell Care India and I am aware that stem cell therapy is the best treatment for ulcerative colitis. They are the greatest healthcare advisors in India, and they help me at every turn. The group was outstanding and gave me the most accurate information. Additionally, the treatment method is simple and efficient. I recommend them to everyone who is suffering from this disorder. If I can get treated then you also. —- Robin Albert, Germany
A quality certificate for stem cell treatment for ulcerative colitis ensures the treatment meets high standards. It confirms that the stem cells are safe, effective, and ethically sourced. This certificate is granted after correct testing and evaluation by health authorities. It gives patients and doctors confidence in the therapy’s safety and reliability. Furthermore, the certification process includes regular inspections and compliance with medical guidelines. By obtaining a quality certificate, stem cell therapy providers demonstrate their commitment to delivering high-quality, trustworthy treatments for Ulcerative colitis, ultimately aiming to improve patient outcomes and safety.
After taking stem cell treatment, there is an important thing you should take which is follow-up. In follow-up, patients visit the doctors for checkups to ensure how progressive stem cell therapy is. The doctor monitors the progress and checks if any side effects start showing. A doctor can do a bunch of tests for you, including blood tests, MRI scans, and many more. These tests will make sure that the effectiveness of the treatment. If a patient witnesses any new symptoms, then it is essential to report it to the doctor. The doctor will suggest you with some of the best physiotherapy and supportive therapy to support your recovery. Maintaining open communication with the doctor helps ensure the best outcomes and allows for adjustments in treatment if needed.
Stem cell therapy is effective in treating a number of medical conditions such as diabetes, neurological disorders, eye disorders, liver disease, lung disease, and many more. This therapy shows positive outcomes for a number of patients and that’s the reason why everyone is choosing this disease over conventional. The therapy is affordable and effective too. However, the success rate is not the same for everyone. Some patients experience long-term benefits. On the other hand, many of them are treated temporarily. Stem cell therapy is still under research and many scientists are trying to make it an effective approach. However, stem cell therapy is not fully prepared but there are no side effects shown to date.
Ulcerative Colitis patients suffered from abdominal pain, diarrhea, and fatigue that interfere with normal life. This chronic inflammatory bowel disease affects the colon and rectum in painful ulcers and great inflammation. This condition’s cause is unknown, yet genetics, immune system failures, and environmental factors are known contributors. It may present with bloody stools, weight loss, and an urgent need to visit the bathroom often, severely impairing quality of life.
Medical management is generally based on medication that reduces inflammation and controls the immune response. The treatment that has been recently found to have the potential for regenerating damaged tissue and modulating the immune system is ulcerative colitis stem cell therapy. A promising breakthrough awaits. Medical approaches target inflammation, while stem cell therapy promises tissue regeneration and immune modulation.
India Provide Top-Notch Medical Facilities To Its International Patients
Strong medical facilities in India, along with its patient care and developing stem cell research capability, can offer foreign patients a promising treatment facility for the proper and safe management of ulcerative colitis. Medical centers have originated places that support dedicated units to deal with stem cell treatment for ulcerative colitis as an effective method for dealing with the disease. The following are some of the major facilities offered by Indian medical institutes:
- State-of-the-Art Diagnostic Centers: Superior imaging and laboratories present excellent diagnostic and treatment planning that provide the patients with the most accurate information about their condition.
- Expert Medical Teams: Doctors, researchers, and the supporting staff are the best professionals in gastroenterology and regenerative medicine. They bring together expert collaboration in formulating a comprehensive treatment plan for each patient.
- Cutting-Edge Stem Cell Laboratories: They have proper, dedicated facilities and quality control measures in place, so that stem cells used in treatment are handled, cultured, and administered in a safe and effective manner.
- Affordability and Value: Compared to most Western countries, India provides an affordable option with no compromise on quality, and thus makes cutting-edge therapies available to a greater international audience.
- Patient-Centric Care: They have multilingual support, personalize the patient coordinators, and give importance to holistic care when international patients travel, including processing of visas, arranging travel to India, among other things.
- Regulatory Compliance and Accreditation: Indian medical centers are registered and compliant with international regulatory requirements. They mostly hold accreditation status with international bodies like JCI.
- Research and Innovation: Ongoing stem cell therapy clinical trials and research ensures that the latest advancements are applied in the treatment of patients with ulcerative colitis, turning the condition into a better one.
Stem cell therapy for ulcerative colitis in India offers international patients a fresh, promising approach to managing the symptoms. With advanced treatments, experienced professionals, and a focus on personalized care, patients can feel confident about choosing India as their destination for a healthier, more hopeful future. People are coming from USA, UK, Europe, Oman, Philippines, Saudi Arabia, UAE, Thailand, Uzbekistan, Yemen, and Kuwait found India a better place for their treatment
Conclusion:
Stem cell therapy offers new hope for people living with ulcerative colitis. It provides a fresh approach when regular treatments fail. Many patients struggle with long-term inflammation. Some deal with repeated flare-ups and discomfort. Stem cell therapy tries to address these deeper issues. It works by calming the immune system. It also supports natural repair inside the colon. These combined actions may bring stronger and longer relief.
Mesenchymal stem cells show great promise in UC care. They can reduce harmful inflammation. They can also help heal damaged tissues. This healing is important for long-term comfort. It also helps stabilize the colon lining. As the colon becomes stronger, symptoms may reduce. Many early studies show good results. These studies highlight better healing and fewer flare-ups. Patients also experience improved daily comfort.
However, more research is still needed. Scientists must confirm long-term safety. They also need to refine treatment methods. Proper guidelines are important for safe use. With more trials, outcomes will become clearer. This will help doctors choose the best approach. Patients will also get better treatment options.
Overall, stem cell therapy brings real potential for ulcerative colitis. It aims to support natural healing and long-term remission. With time and research, it may become a reliable future treatment. It offers hope for a healthier and more stable life.